Simulation has been a key component of medical education experienced by today’s clinicians as medical students or doctors in training. The days of first learning new skills on real patients based on a ‘see one, do one, teach one’ model are thankfully long behind.
As the complexity of medicine has increased along with technological advancements in medical care there has been an increasing need to learn and practice new skills in a safe and protected environment before moving on to real patients.
Medical simulation training aims to recreate real-life clinical scenarios, allowing learners to practice and master skills resulting in improved patient safety and ensuring the highest standards of patient care.
Traditional Simulation
The traditional approaches to simulation in medicine has taken many forms as considered below:
Standardized Patients
Uses actors or ordinary people trained to portray the symptoms and signs of a particular medical condition. These ‘patients’ interact with students, allowing them to practice history taking, physical examination, and communication skills in a controlled environment.
This provides a safe space for students to make mistakes, learn from them, and improve their clinical skills without any real-world consequences.
Manikin Based Simulation
Manikins are life-sized models that can range from low fidelity (showing basic surface anatomy) to high fidelity (having advanced features like palpable pulses and reactive pupils). They are the mainstay of life support course training such as Advanced Cardiac Life Support which uses CPR manikins, allowing students to practice chest compressions and airway management.
Manikin based simulations are particularly useful for practicing emergency scenarios and can be used to simulate team-based emergency care.
Role-playing
Students take on roles in a simulated medical scenario to practice communication and decision-making skills. A scenario could involve breaking bad news where one student might play the role of a doctor, another a patient, and a third as a concerned relative with the focus being learning empathetic communication.
This avoids the need for individuals trained to portray a patient and allows experiential learning for all students in the group.
Skills Trainers
These are models designed to allow practice of a specific medical procedure or skill. They can be as simple as a suture pad that mimics human skin allowing students to practice suturing wounds to complex models simulating performing a cesarean section.
Skills trainers provide reasonably realistic tactile feedback allowing students to gain the motor skills required and to gain confidence in performing the procedure.
High Fidelity Task Trainers Simulation
These are more complex versions of skills trainers that are designed to simulate a portion of a complex procedure, such as a laparoscopic surgery trainer simulation, where clinicians can practice performing minimally invasive surgery guided only by video feedback.
This provides tactile motor training but also the skills of coordinating movement of instruments in 3D guided only by 2D video.
Hybrid Simulation
Combines elements from different simulation modalities to create a more comprehensive learning experience. This can involve a ‘patient’ wearing prosthetics to mimic certain medical conditions or to allow procedures to be practiced.
This offers a multi-faceted learning experience by placing clinical examination or procedural skills in the context of a living patient which requires simultaneous use of communication and practical skills.
Computer-based simulation
These are software applications that focus on decision making by presenting a clinical scenario, allowing students to choose which investigations and treatments to perform.
These computer-based simulations are flexible and allow for self-paced learning but lack the experience of immersion. With more complex scenarios, students can revisit them to improve their decision making until they master the topic.
Extended Reality Simulation
Computer based simulations represented the dawn of utilizing advancements in technology to enhance medical education and could be considered the foundation of technology enhanced learning.
Over the last few years, there has been rapid expansion and development of Technology Enhanced Learning, often in the form of Extended Reality. All these evolving immersive technologies are often grouped together but there are distinct types as outlined below:
Augmented Reality (AR)
AR superimposes digital information on to the real world, in the form of images, diagrams, or video. This can be overlaying anatomical information onto a patient’s body so that students can point a tablet or AR glasses at a body region and then be presented with underlying organs, muscles, or bones. This offers a dynamic and interactive way to learn the complexities of human anatomy.
Virtual Reality (VR)
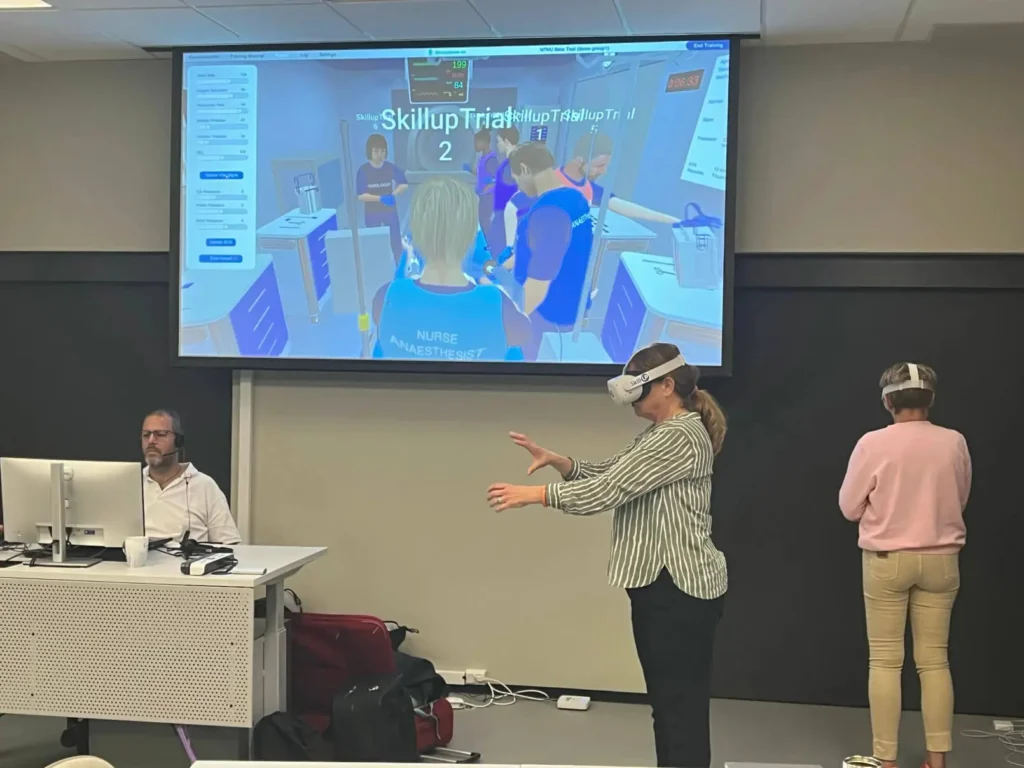
VR immerses the learner into an entirely simulated environment, via a headset that tracks their motion, allowing them to move and interact within the virtual space. In medical education VR offers enormous possibilities, ranging from straight forward patient scenarios to complex surgical simulations. It offers an immersive but risk-free environment for students to gain clinical experience without mistakes having real world consequences.
Mixed Reality (MR)
MR is a mix of both AR and VR as it places virtual objects to the real world, allowing users to interact with both simultaneously.
It can be used for surgical simulation, allowing clinicians to practice procedures on virtual organs while using real surgical instruments.
Comparison of extended reality simulation with traditional simulation
Many other sectors, including aviation and the military, have already harnessed the potential of VR based simulation training. Within healthcare, many studies have demonstrated the efficacy of VR in providing training over a wide range of topics and skills.
It is worth considering and contrasting the roles, benefits, and limitations of traditional and extended reality simulation to better understand the future of medical education:
Cost
Traditional manikins or skills trainers can be expensive, even at a basic level, but especially the high-fidelity versions. Until recently, the initial setup cost for extended reality simulation could be high, however, an increasing number of subscription-based VR training solutions running on standard commercially available headsets can be available at a fraction of the cost required to operate and maintain traditional manikin-based simulations. In the long-term, VR simulation can be cost-effective as they can simulate and repeat a multitude of scenarios without additional equipment and expense.
Versatility
Extended reality can offer a wide range of scenarios, from teaching basic anatomy to simulating complex team-based life support training. Software updates can be easily installed, making them adaptable to the evolving needs for medical simulation. In contrast, manikins are limited in the range of scenarios they can depict.
Tactile Feedback
One advantage of training on a manikin-based simulator is the tactile feedback it provides. When practicing procedures like CPR or intubation, sensory feedback and motor coordination are important aspects. While VR and AR focus more on the visual and auditory aspect, MR can bridge this gap by integrating haptic feedback.
Virtual reality still has much to offer in practical skills training as physically performing the skill is just one aspect of learning a new clinical skill. Knowing why to do it, when to do it, the correct sequence of steps, how to assess if it has been successful and the identification and management of complications are all important aspects of learning which can be addressed in VR.
Space
High fidelity manikin-based simulations usually require a dedicated space, often in a purpose-built simulation center. In contrast, extended reality is more mobile and not limited to physical space or location.
Engagement & Immersion
Immersive technologies are more engaging for trainees and can offer a gamified approach to learning, making complex medical topics more memorable.
International Collaboration
Virtual reality training makes it easy to bring together a team from around the world, for example, an instructor in Norway can facilitate a team-based simulation with learners from Europe, Asia, or anywhere else in the world with wifi connection. With this comes the potential to revolutionize global healthcare education.
Safety & Resilience
Virtual simulations eliminate the need for face-to-face teaching. In the wake of pandemics, this advantage can reduce risk and offer resilience to training in the face of future events.
Unlike traditional simulation, VR offers an immersive experience where learners are placed within an interactive simulated environment improving their engagement and fostering experiential learning. Skillup VR medical simulation is an advanced solution that allows learners to practice critical skills such as communication, decision making and teamwork in a realistic clinical environment on demand without geographic barriers.
Harnessing the potential of VR medical training promises a future where medical simulation is more realistic, immersive, interactive, and globally accessible, to ensure that the next generation of healthcare professionals are equipped to meet the challenges and escalating complexity of evolving modern medicine.